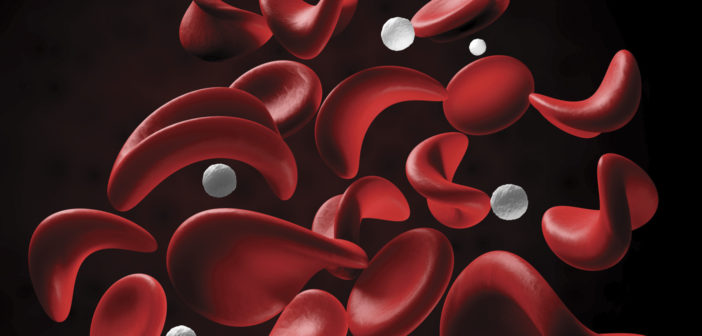
Sickle Cell Disease (SCD) is an inherited condition that leads to abnormal hemoglobin within the Red Blood Cells (RBCs). The RBCs with sickle hemoglobin become rigid when oxygen concentration becomes low. When this happens, the RBCs are unable to move through very small blood vessels and tissues lack adequate oxygen. The clogging of blood vessels with very rigid red blood sickle cells leads to painful episodes and other very serious complications.
In the U.S., SCD affects approximately one in 400 African Americans – one in 12 African Americans have the sickle cell trait. Persons of other ethnicities, like Latinos, are less affected. In 1987, the State of Michigan added a test to diagnose SCD to the newborn screening test, which determines whether the newborn is normal, has sickle cell trait, or SCD. Therefore, individuals with SCD are diagnosed at birth before they start having complications and crisis.
Acute Complications of SCD (Sickle Cell Crisis)
Chronic Anemia: This means a low number of RBCs and hemoglobin that leads to a feeling of tiredness and fatigue. Blood transfusion is used to treat severe cases.
Pain: The most common complication of SCD, pain can occur anywhere in the body. This is managed by prompt initiation of hydration, rest and pain medications either at home for mild cases, or in the hospital for moderate to severe or prolonged cases.
Delayed Growth: Patients with SCD may be smaller than peers and puberty may also be delayed.
Gallstones: This is a very common complication of SCD, with symptoms including recurrent right upper abdominal pain and increasing jaundice. Ultrasound of the abdomen is used to confirm this complication.
Bedwetting: A very common problem in children with SCD due to the kidneys’ inability to concentrate urine.
Other complications include vision disturbances, leg ulcers or priapism (painful penile erection).
In the U.S., SCD affects approximately one in 400 African Americans – one in 12 African Americans have the sickle cell trait.
Life-threatening Complications of SCD
Infections: Children with SCD are at increased risk for severe bacterial infections. This risk is less in adults. A child with SCD with fever should be promptly evaluated by a physician.
Splenic Sequestration: Sickled red blood cells become trapped in the spleen, causing it to enlarge and affect function. Symptoms include irritability, weakness, and pain on the left side of the abdomen. This requires emergency medical attention.
Strokes: Risk of stroke is high in individuals with SCD. Eighty percent of strokes occur before age 20. This also requires emergency medical attention.
Acute Chest Syndrome (ACS): This resembles pneumonia, and risk is increased in people with asthma. ACS is the most common cause of death in adults with SCD.
Health Maintenance
- Care Coordination: This requires cooperation between the primary care physician and hematologist.
- Prevention of Infections: Use of penicillin prophylaxis is given twice daily in children with SCD until the age of five years. Individuals with SCD should receive all recommended immunizations and be vaccinated against bacteria called streptococcus pneumoniae.
- SCD also increases risk of adverse pregnancy outcome. Reproductive health counseling should be offered and all pregnancies should be considered high risk.
- Children with SCD aged 2-16 are screened annually with Transcranial Doppler (TCD) to determine stroke risk.
- Exposure to extreme cold or warm temperatures may initiate a pain episode.
Treatment of SCD
- The ideal treatment for SCD should show clinical benefits, have few side effects and must be safe with few long-term associated risks. Hydroxyurea was approved by FDA in 1998 for the treatment of severe SCD in adults. Currently, it is used in children and adults with SCD as a disease-modifying agent. This is an oral medication given once daily to prevent SCD crisis.
- L-glutamine is given orally to prevent pain crisis.
- Red blood cell transfusion is used to treat acute complications and prevent chronic complications.
- Bone marrow or stem cell transplant is the only available treatment that offers curative potential. Only 15-20% of children with SCD are likely to have a matched sibling donor for transplant.
- Gene therapy and other newer therapies in the early phase of development.
In the not so distant future, the palliative treatment and symptom relief approach to SCD will be replaced with curative approaches.