For many people, the thought of having surgery is terrifying. So, My City Wellness has “scrubbed in” with talented local surgeons as they performed a variety of procedures – a peek behind the curtain, if you will. Our sincere thanks to Michael Engel, DO; Mustafa Hassan, MD and Niraj Parikh, MD for their gracious cooperation in creating this ongoing special section.
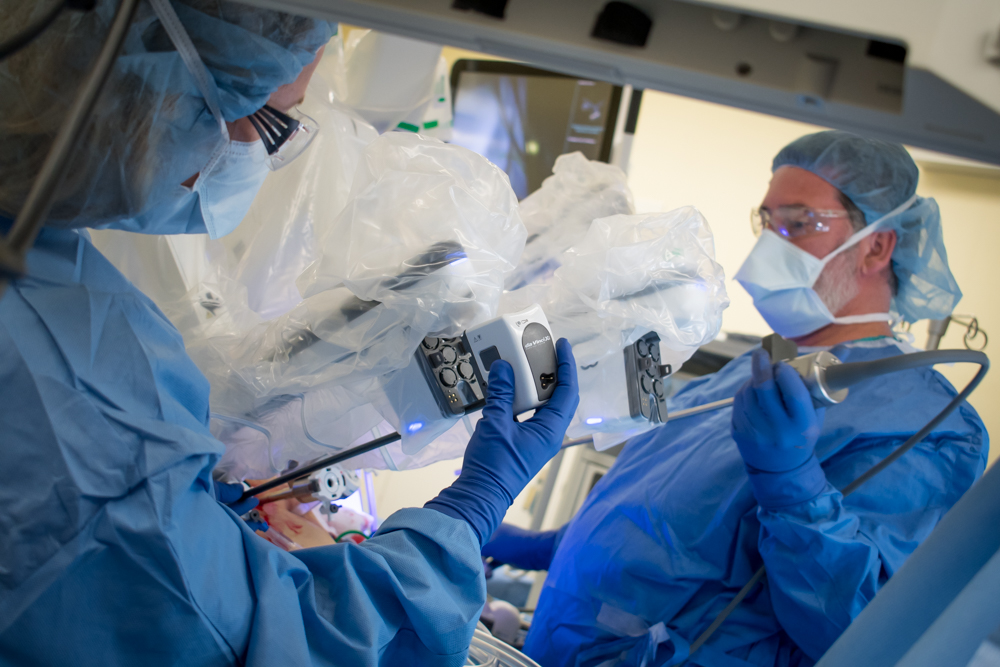
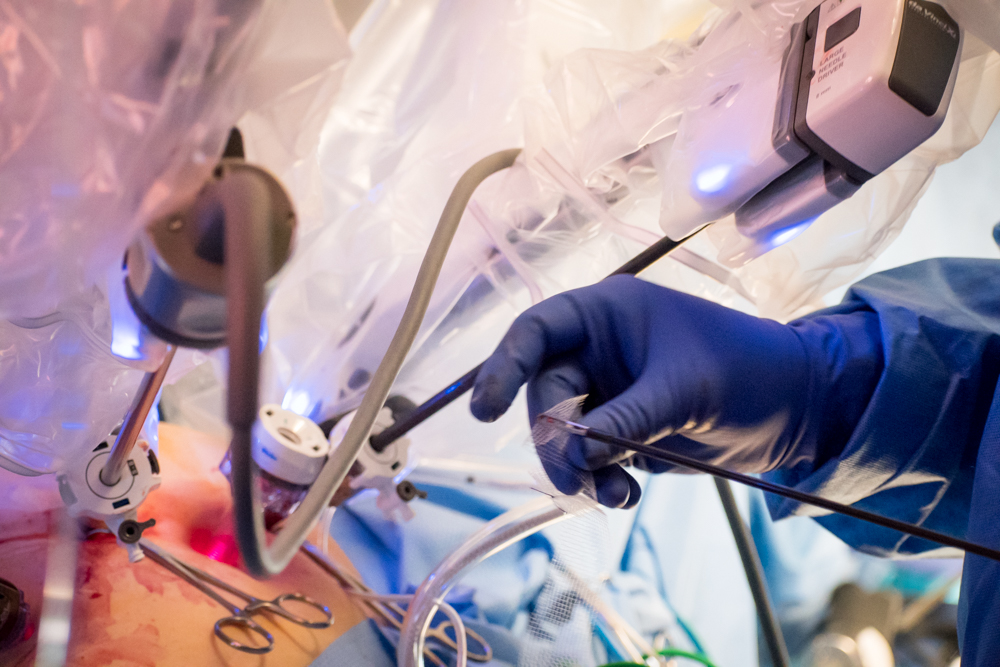
 Robotic da Vinci® Sacrocolpopexy for
Robotic da Vinci® Sacrocolpopexy for
Vaginal Vault Prolapse
McLaren Flint
Michael Engel, DO
Board-certified in Obstetrics and Gynecology, Dr. Engel has 20 years of experience serving patients. He attended medical school at Michigan State University College of Osteopathic Medicine and completed his internship and residency in OB/GYN at McLaren Macomb, where he also served as chief resident. Dr. Engel has significant experience in laparoscopic surgery, reconstructive pelvic surgery, and daVinci® robotic procedures. He has served as a hospitalist in labor and delivery, as well as teaching and mentoring resident physicians. To date, he has performed over 150 robotic-assisted gynecologic procedures, including hysterectomies and sacrocolpopexies.
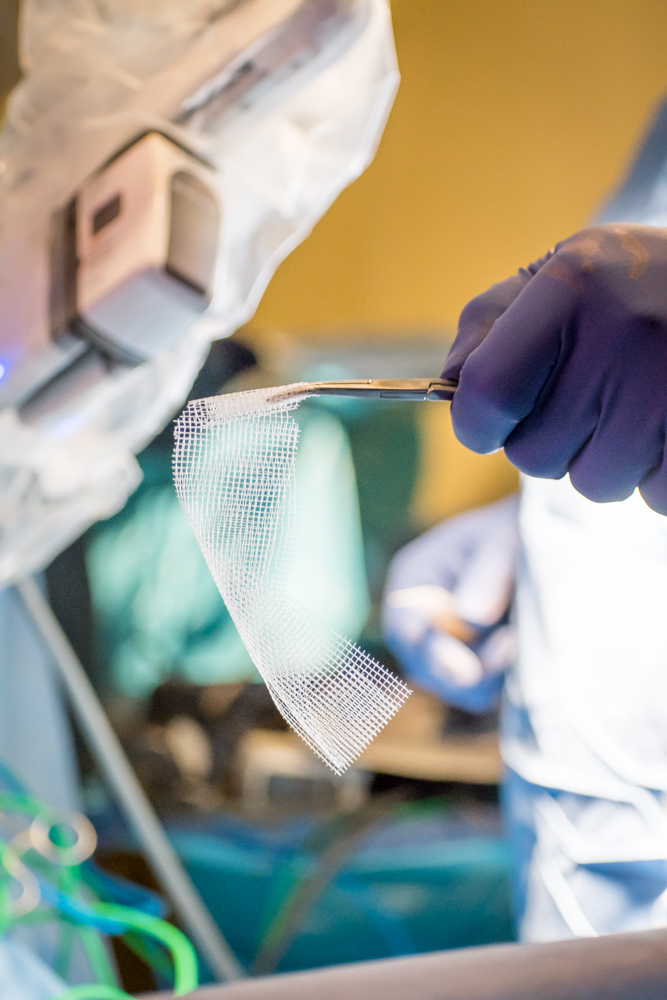
This procedure is performed to correct pelvic floor dysfunction including incontinence, and vaginal vault and/or rectal prolapse through the use of mesh that holds the vagina in the correct anatomical position.
Each year in the U.S., 120,000+ cases of uterine and vaginal vault prolapse are surgically treated. Prolapse (or falling) of any pelvic floor organ (vagina, uterus, bladder or rectum) occurs when the connective tissues or muscles within the body cavity are weak and unable to hold the pelvis in its natural orientation.
The weakening of connective tissues accelerates with age, after child birth, with weight gain and strenuous physical labor. Women experiencing pelvic organ prolapse typically have problems with urinary incontinence, vaginal ulceration, sexual dysfunction and/or having a bowel movement.
Sacrocolpopexy is a term that literally means “lift the vagina to the pelvic bone” (sacro – the portion of the back bone in the pelvis; colpos – vagina; pex – to suspend or lift up). This procedure can also be performed along with a hysterectomy to treat uterine prolapse and provide long-term support of the vagina. Long-term cure rates are about 90 percent, as this procedure provides complete support to the vagina, especially to the top/front of the vagina that is the area most likely to prolapse.
The robotic assistance technology used for this procedure allows for more intricate movements than possible with the surgeon’s own hands, because the tools are smaller with a greater degree of maneuverability. Robotic surgery is minimally invasive, meaning the only incisions needed are typically less than an inch long, made to create an entry point for the laparoscopic tools. The surgeon performs the procedure using high-definition cameras, allowing for detailed magnification of the site.
This is typically an outpatient procedure. Women who have this surgery usually require a one- to two-week recovery time, and some can return to work in two to three weeks. Dr. Engel has performed over 150 total robotic procedures.
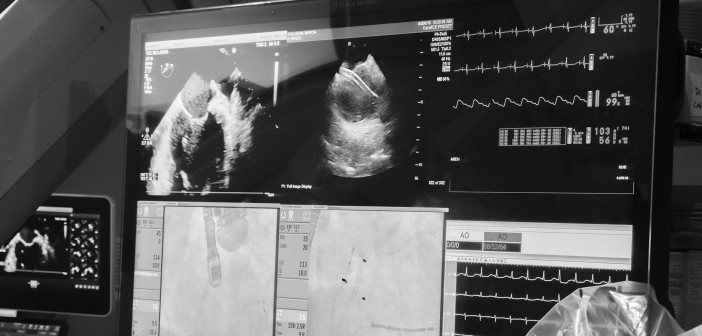
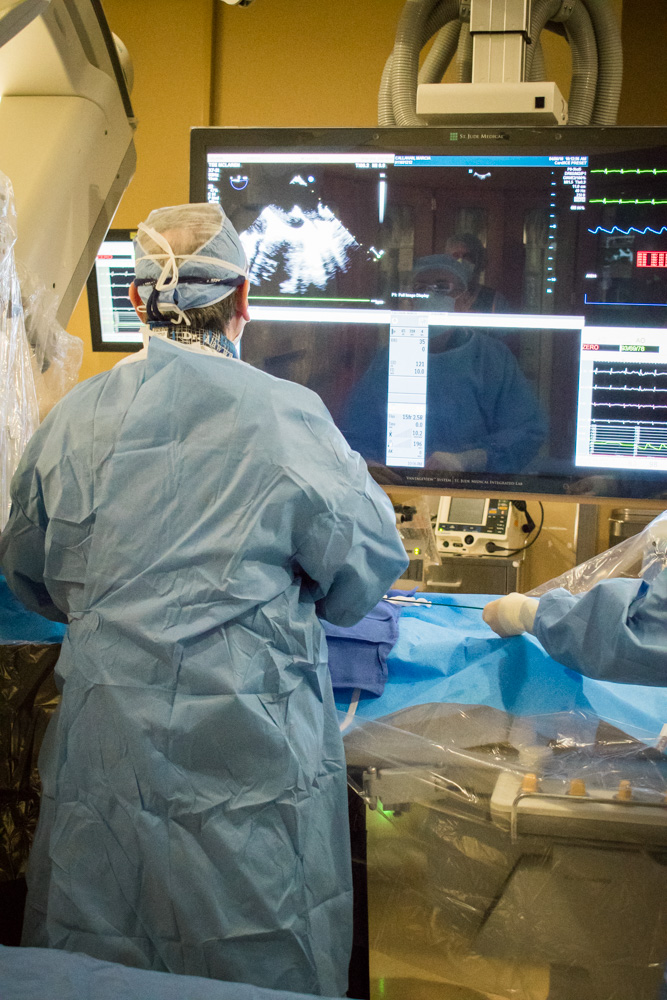
Percutaneous Closure of the Left Atrial Appendage using the WATCHMAN Device Cath Lab, McLaren Flint
Mustafa Mahmoud Hassan
MD, FACC, FHRS
Board-certified in Cardiovascular Disease, Clinical Cardiac Electrophysiology and Internal Medicine, Dr. Hassan is a cardiologist in Flint, and is affiliated with multiple hospitals in the area, including Hurley Medical Center and McLaren Flint. He received his medical degree from University of Gezira Faculty of Medicine and has been in practice for more than 20 years.
The WATCHMAN Device is a permanent heart implant that effectively reduces the risk of stroke, without the risk of bleeding that can come with the long-term use of Warfarin (the most common blood thinner). In addition, WATCHMAN can eliminate the regular blood tests and dietary restrictions that come with blood thinner use. This procedure can reduce the risk of stroke in patients who have atrial fibrillation (AFib) not caused by a heart valve problem (also known as non-valvular AFib). Any person considering this procedure must be evaluated to determine whether they are a candidate.
The technology that makes the WATCHMAN device innovative and effective is that it is designed to fit, and close, the left atrial appendage. It is small enough to be done through a small incision in the skin (percutaneously), in the groin of the leg. The procedures takes place in a heart catheterization lab and the patient is under general anesthesia.
Following the procedure, the patient will need to stay in the hospital overnight. They cannot do strenuous activity for one week and will remain on blood thinners for six weeks.
The program started late last year, and Dr. Hassan is one of four specialists implanting the WATCHMAN device. The McLaren group has performed 49 procedures to date. The current success rate of this procedure is 95 percent.
 Bronchoscopy with Endobronchial Ultrasound and Navigational Bronchoscopy
Bronchoscopy with Endobronchial Ultrasound and Navigational Bronchoscopy
Hurley Medical Center
Niraj Parikh, MD
Pulmonary / Critical Care / Sleep Doctor
Dr. Parikh is board-certified in Internal Medicine, Pulmonary, Critical Care and Sleep Medicine. He did his Fellowship in Pulmonary, Critical Care and Sleep Medicine at Henry Ford Hospital, Wayne State University in Detroit, MI. He completed medical school at Sardar Patel University, India and his Internal Medicine Residency at Sinai-Grace Hospital, Detroit Medical Center. Dr. Parikh is a Clinical Assistant Professor in the Department of Medicine at Michigan State University. He joined Pulmonary Associates, P.C. in Flint, MI August 2016 where he currently practices. He splits his time between clinic patients, sleep lab, hospital rotations, Intensive Care Unit and performing numerous procedures. He is on staff at Hurley Medical Center and McLaren Regional Medical Center in Flint, MI.
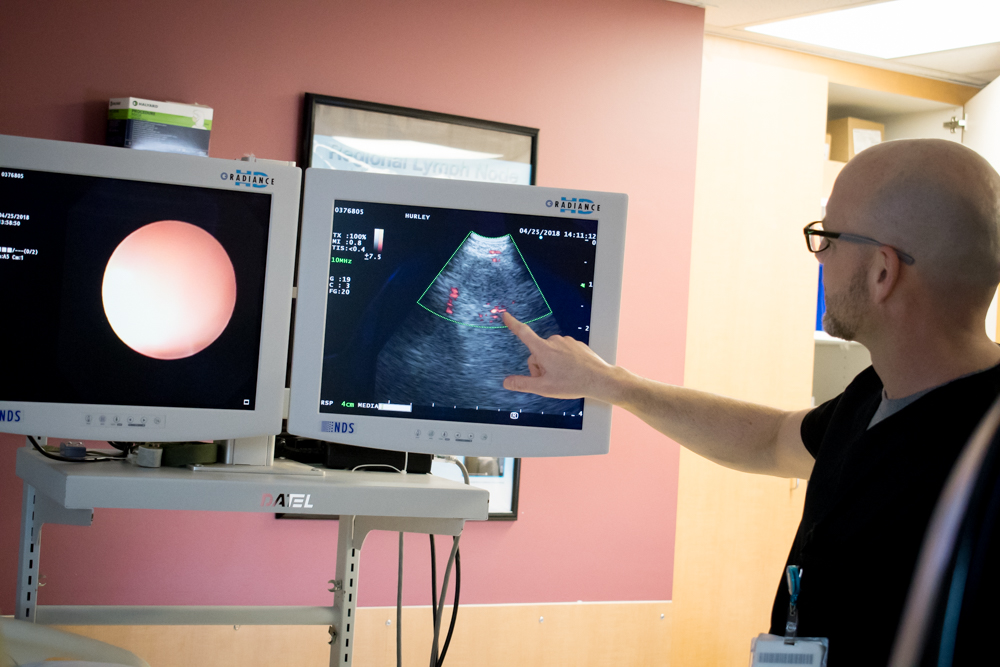
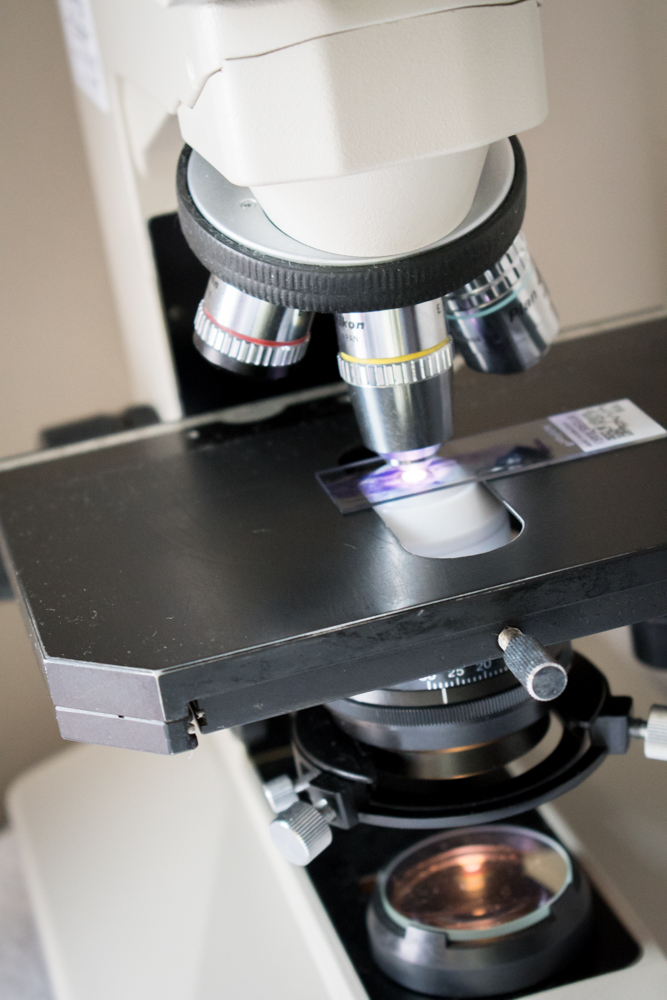
Bronchoscopy with EBUS (endobronchial ultrasound) is a minimally invasive procedure used to diagnose different types of lung disorders, including inflammation, infections or cancer. Performed by a pulmonologist, EBUS bronchoscopy uses a flexible tube that goes into your windpipe and lungs through the mouth. Similar to, though smaller than the device used during a colonoscopy, the EBUS scope has a video camera with an ultrasound probe attached to create a local image of your lungs and nearby lymph nodes in order to accurately locate and evaluate areas seen on x-rays or imaging that need a closer look.
This procedure can be done on an outpatient basis, where patients can come in the morning and go home by noon. If cancer is detected, the diagnosis and staging information is available at the same time, saving patients from needing additional procedures.
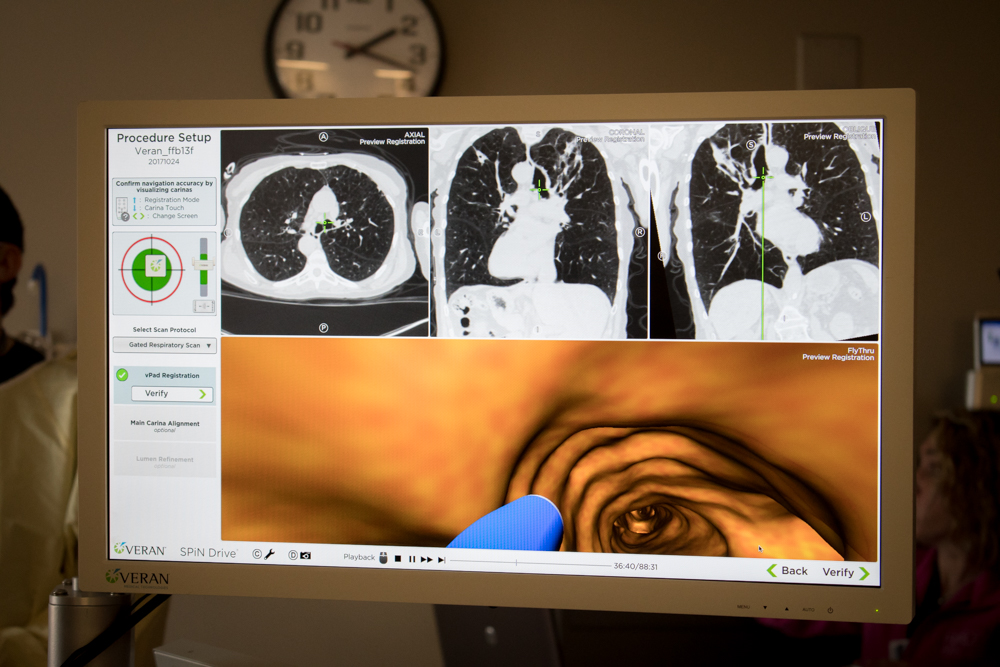
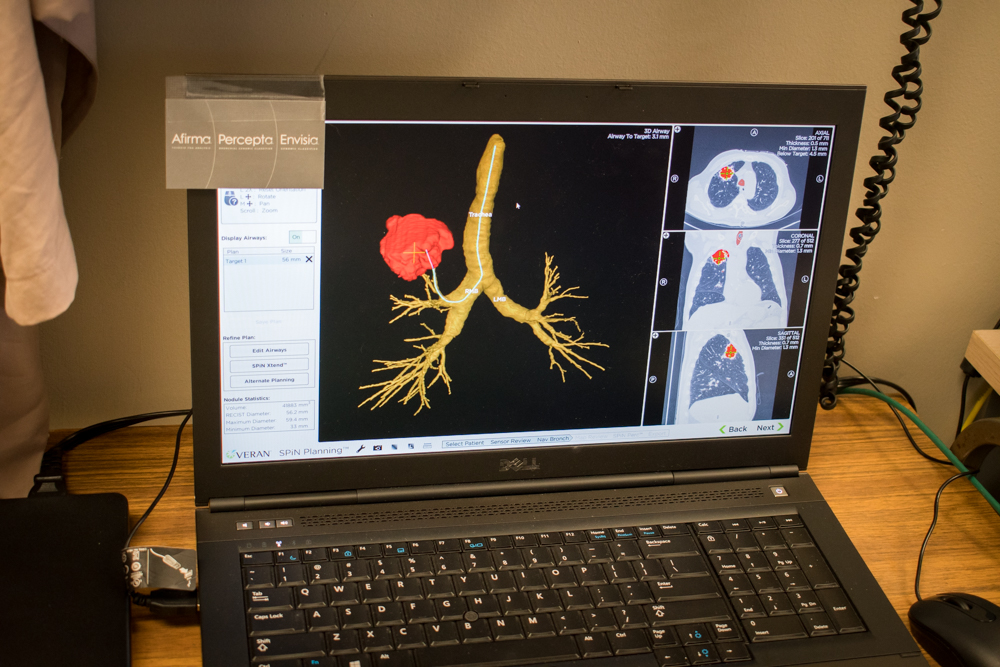
Navigational bronchoscopy allows identification of a peripheral lung nodule based on CT scan imaging and, subsequently, a biopsy of lung lesions that would normally be inaccessible via traditional bronchoscopy. The procedure has similar advantages of being able to schedule the procedure as an outpatient and making the diagnosis with minimal risk of complications.
Using an innovative technology similar to GPS, the procedure starts with a CT scan of the chest and subsequent identification of a lung lesion, and the technology creates a map on how to reach the lesion.
Anesthesia is used during this procedure and thus, patients are typically sleepy for the rest of the day after the procedure. Most can go home the same day and return to work the next day. This is still an invasive procedure and patients cannot be on certain blood thinners. All precautions are taken to modify a patient’s medications so they can successfully have this procedure.
Dr. Parikh’s physician group has done both of these procedures more than hundreds of times.
Photography by Jennifer Hodney